Allergies are among the most common chronic health conditions globally, affecting millions of people across all ages and environments. They occur when the body’s immune system reacts inappropriately to substances that are harmless for most individuals. These reactions can vary from mild irritation to severe, life‑threatening episodes. In this detailed medical overview, we’ll explore what allergies are, how they develop, why certain people are more at risk, and how they are diagnosed and treated. You’ll also find clear explanations, tables for quick reference, and links to high‑authority health sources that deepen your understanding of this complex immune‑related condition.
What Is an Allergy? Immune System Basics
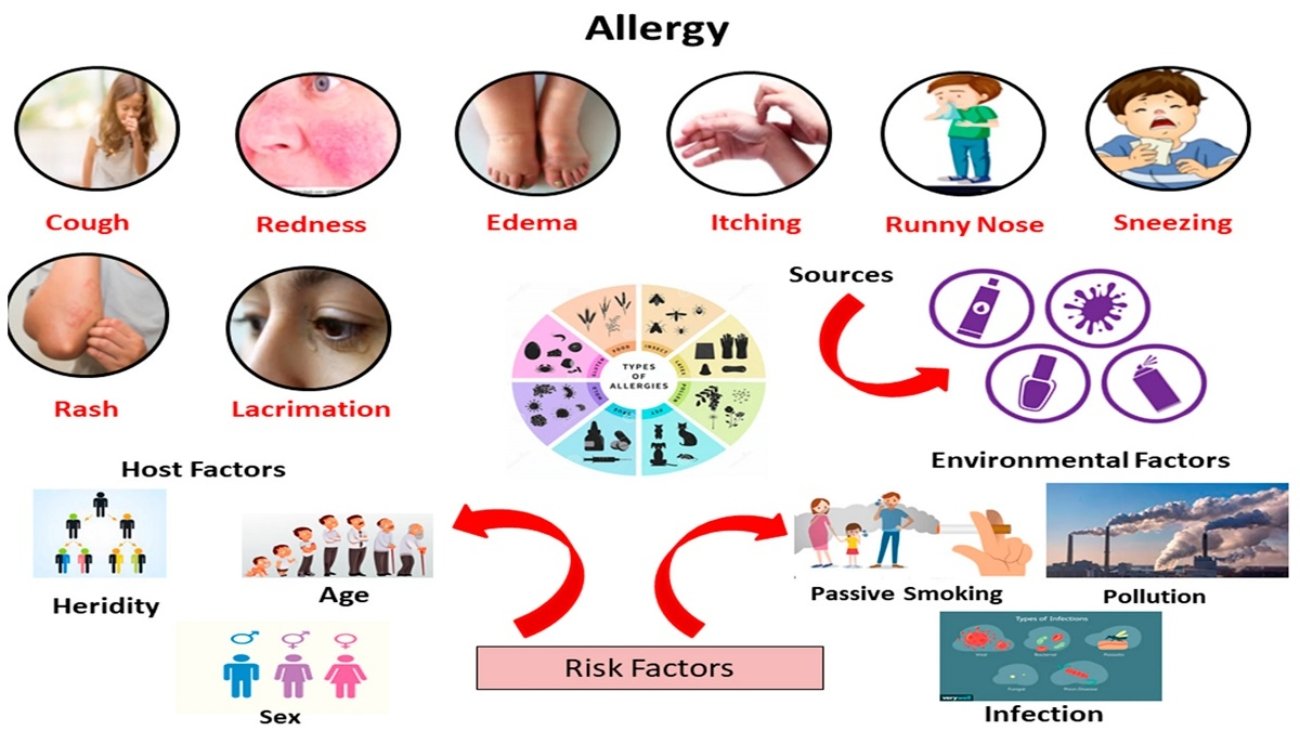
Allergies arise when the immune system mistakenly identifies an otherwise harmless substance as dangerous. These substances are known as allergens, and exposure triggers an immune response featuring a class of antibodies called immunoglobulin E (IgE). During first exposure, the immune system becomes sensitized to the allergen. On subsequent exposures, the IgE antibodies mobilize immune cells to release inflammatory chemicals such as histamine. This cascade produces classic allergy symptoms like itching, sneezing, swelling, and, in severe cases, systemic reactions. This mechanism explains why symptoms occur across different organs like the skin, airways, eyes, and digestive tract.
For deeper immunological context, you can visit the Mayo Clinic overview of allergy symptoms and causes which explains these processes clinically and symptomatically.
Types of Allergens and Common Triggers
Allergens can be present in the air, in foods, on surfaces, or even in medications. The main categories include:
Airborne Allergens
Airborne allergens are among the most pervasive triggers worldwide. These include:
- Pollen from trees, grasses, and weeds.
- Dust mites found in home dust.
- Mold spores thriving in damp indoor environments.
- Animal dander from pets like cats and dogs.
These allergens are frequently implicated in allergic rhinitis (hay fever), which causes symptoms such as nasal congestion, sneezing, and itchiness. Indoor and outdoor exposures both contribute to persistent or seasonal symptoms.
Food Allergens
Food allergies involve immune reactions to specific dietary proteins. The U.S. Centers for Disease Control and Prevention (CDC) data shows that in 2021 about 5.8% of children had diagnosed food allergies, which is part of the broader spectrum of allergic conditions in pediatric populations.
Foods commonly implicated include:
| Common Food Allergens | Typical Reactions |
|---|---|
| Peanuts | Severe anaphylaxis possible |
| Tree nuts | Often triggers multiple allergies |
| Shellfish | Common adult allergen |
| Milk and Eggs | Frequent in children, sometimes outgrown |
| Wheat and Soy | Can cause GI and skin reactions |
| Sesame | Increasingly recognized allergen |
Data suggests these foods account for the majority of clinically significant reactions.
Contact Allergens and Other Triggers
Direct skin contact with substances like latex, metals (e.g., nickel), cosmetics, or fragrances can trigger allergic dermatitis. This skin inflammation reflects the immune system’s reaction at the surface level.
Insect venoms from bees or wasps and specific medications like penicillin can also provoke systemic allergic responses, sometimes severe enough to cause anaphylaxis.
Common Allergy Conditions Explained
Allergies present in diverse forms depending on the organ systems involved. Here’s a structured look at major clinical categories:
Allergic Rhinitis (Hay Fever)
This is the most widely recognized type of allergy, especially in seasonal patterns. Symptoms include:
- Sneezing and nasal congestion
- Runny nose
- Itchy nose, throat, and eyes
- Fatigue due to disrupted sleep
This condition often coincides with exposure to pollen, dust mites, or mold and can be perennial (year‑round) or seasonal.
Food Allergy Reactions
Food allergies can affect the digestive system, skin, and respiratory passages. Severe reactions, known as anaphylaxis, involve difficulty breathing, low blood pressure, and potential collapse. Quick treatment with epinephrine is often life‑saving.
Skin‑related Allergies
Hives, eczema, and contact dermatitis fall under this category. They typically manifest as itchy, inflamed patches of skin triggered by contact with allergens.
Asthma and Allergic Components
Asthma is a chronic respiratory condition often linked to allergic reactions, particularly in individuals with allergic rhinitis or atopic tendencies. Asthma involves airway inflammation and bronchoconstriction, which can be exacerbated by allergens like pet dander and pollen.
How Common Are Allergies?
Allergic conditions are pervasive worldwide, affecting significant portions of both adult and pediatric populations.
Prevalence in the United States
- Over 50 million Americans suffer from allergies annually.
- Approximately 30% of adults and 40% of children report some form of allergy.
- Seasonal allergic rhinitis (hay fever) affects up to 26% of adults and 19% of children in the U.S. alone.
Global Estimates
Worldwide, estimates indicate that 30–40% of people have one or more allergic conditions, with allergic rhinitis affecting between 10% and 30% of the population.
Food Allergy Prevalence
Food allergies affect up to 10% of the global population, with higher rates in children compared to adults. Cow’s milk, eggs, peanuts, and tree nuts are among the most common triggers globally.
Risk Factors: Who Gets Allergies?
Several factors increase susceptibility to allergic reactions:
- Genetic predisposition: Children with allergic parents have higher risk.
- Early environmental exposures: Hygiene and diet patterns in infancy influence immune development.
- Living conditions: Urban environments and pollutant exposure may elevate risk.
Additionally, lifestyle and dietary changes over decades have correlated with rising allergy rates, especially in industrialized nations.
How Are Allergies Diagnosed?
Accurate diagnosis helps tailor effective treatment plans. Common diagnostic tools include:
Skin Prick Test
Small amounts of potential allergens are placed on the skin surface and reactions are observed.
Specific IgE Blood Tests
These measure the amount of allergen‑specific IgE antibodies present in the blood, guiding identification of trigger substances.
Oral Food Challenges
Under strict medical supervision, suspected food allergens are introduced to confirm or rule out allergy.
Allergy testing should be interpreted by trained clinicians, ideally allergists or immunologists, to ensure accurate diagnosis and management.
Management and Treatment Strategies
While most allergies cannot be fully cured, symptoms can be controlled and complications reduced through evidence‑based strategies.
Pharmacologic Treatments
Medications include:
- Antihistamines to relieve sneezing, itching, and runny nose
- Nasal corticosteroids for severe nasal symptoms
- Decongestants for short‑term relief
- Leukotriene inhibitors for airway inflammation
These therapies address symptoms but may not change the underlying immune response permanently.
Immunotherapy
Allergen immunotherapy (allergy shots or sublingual tablets) gradually exposes the immune system to increasing amounts of allergen proteins. Over time, this process may reduce sensitivity and frequency of reactions. It’s one of the few interventions that can modify the immune system’s response rather than just mask symptoms.
Avoidance and Environmental Controls
Practical steps include:
- Monitoring local pollen forecasts and minimizing outdoor exposure on high‑pollen days
- Using HEPA filters and maintaining clean indoor air
- Regular washing of bedding and vacuuming with allergen‑reducing techniques
- Avoiding foods or substances known to trigger reactions
Emerging Insights: Prevention and Early Exposure
Newer pediatric guidelines recommend early introduction of allergenic foods such as peanuts during infancy to help reduce the risk of developing food allergies. Real‑world evidence now shows significant declines in peanut allergy rates following these early‑feeding guidelines, heralding a potential shift in allergy prevention strategies.
Summary of Key Allergy Concepts
Allergies reflect a complex interaction between immune defenses and environmental exposures. They are widespread, lifelong conditions in many individuals, but with precise diagnosis and multi‑modal management, symptoms and quality of life can be greatly improved. Integrating both medical treatments and lifestyle adjustments supports strong overall immune health and day‑to‑day comfort.
This information is for educational purposes and does not replace professional medical advice. Always consult your Doctor.

What’s up everyone! If you’re attempting to understand what season you are or which colors suit your skin tone best, tools like the color analysis pro app and online quizzes can be a superb start. For example, if you have a porcelain skin tone with yellow undertones or olive skin, exploring palettes like deep summer or light spring color palette might definitely help refine the best colors for you. It’s interesting how seasonal color analysis uses skin tone charts, vein tests, and undertone observations—like blue veins or reddish undertones—to establish flattering color palettes.
For those interested in deep summer color analysis, the palette often includes subtle and cool shades which suit yellow skin tone females or people with an amber skin tone. You can also access free color analysis and hair color simulators online to practice before committing. If you want to investigate seasonal color palettes and find out what colors enhance pale skin, yellow undertone, or olive skin, view amber skin color for comprehensive charts and tips!